Some users may experience temporary issues accessing parts of the site. Thanks for your patience.
- Office Hours Mon - Fri 9:00 am – 4:00 pm EST
Why do we ask for the patient’s TMJ history as a part of our complete exam? Particularly, why do we ask a history of open or closed lock?
 Our main goal of this question is to have a better understanding of the patient’s TMJ status.
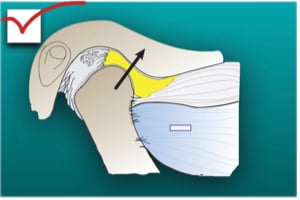
Our main goal of this question is to have a better understanding of the patient’s TMJ status.So how does this information give you a better picture of someone’s TMJ? In order to answer that, we need to understand what is going on at the joint level when a patient experiences open or closed lock. In a normal healthy temporomandibular joint, condyle, disc, muscle, and ligament work harmoniously for the proper mandibular movement. The disc is firmly attached to the lateral and medial poles of the condyle. It is extremely rare that a patient would experience frequent open or closed lock in structurally healthy joints.
 The first situation is an accident involving head trauma.
The first situation is an accident involving head trauma.For example, a car accident with head flexion and extension (whiplash). Sudden trauma injury to the TMJ can mechanically displace the disc forward and/or stretch or tear retrodiscal tissue. This introduces bleeding into the joint space and causes inflammation and swelling.
If we don’t address this in a timely manner, it becomes a chronic situation and there is a permanent structural change. When it becomes a chronic condition, the muscle fiber of the lateral pterygoid attaches to the anterior portion of the disc, which causes it to become foreshortened and fibrous. Retrodiscal tissue can also become fibrous, as well.
Generally, internal derangement of the TMJ starts at the lateral pole of the condyle. Incoordination of the superior lateral pterygoid and elevator muscles stretch the posterior discal ligament and the lateral half of the disc forcing it to become anteriorly displaced. As it progresses further through the stage of derangement, it involves the medial pole and medial half of the disc is displaced anteriorly.
For example, the patients cannot close their teeth together after a lengthy procedure like wisdom teeth extractions or root canal treatment. It usually happens to patients who have an existing intracapsular TMJ disorder. When they open for a long period of time, damaged discs tend to displace forward and blood accumulates in the tissue behind a condyle. This prevents the condyle from fully seating in the glyenoid fossa.
No. It’s a specialty patient. It is an important sign for us to get a correct diagnosis of the TMJs prior to any definite treatment.
We need to perform a thorough complete exam with possible imaging to find out if there is an intracapsular and/or extracapsular joint problem.
Temporomandibular disorder is a progressive disease. Recognizing signs before permanent structural damage to the TMJ is key. Having a clear picture of the TMJ is a good start to delivering predictable dentistry that all our patients deserve because TMJ is the structural foundation of occlusion.
To learn more about TMD diagnosis and treatment, consider a course in our TMD and Facial Pain Curriculum.
ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry.
Concerns or complaints about a CE provider may be directed to the provider or to the Commission for Continuing Education Provider Recognition at ADA.org/CERP.