
Hygiene: A Day in the Life of Dr. Dawson’s Hygienist
Nearly 40 years ago, I started my career as a dental hygienist for Drs. Pete Dawson and Pete Roach. Now, I currently practice in the office of Dr. Kim Daxon, previously owned by Dr. Dawson and Dr. Pete Roach. To ensure that the doctor’s time with the patient is maximized, I make sure that I look for several things in every hygiene appointment. Having an understanding of complete dentistry is the viewing and understanding the masticatory system (Temporomanidbular joints, muscles, teeth and periodontal structures) as a whole and treating any issues.
Complete Dentistry is understanding and recognizing signs of instability.

TMJ: Limited range of motion, joint noises, jaw asymmetry, midline discrepancies, anterior open bite, posterior open bite and bite changes.
Muscle: Headaches, jaw quivering, jaw fatigue, limited range of motion and tenderness in muscle.
Occlusal and teeth: Wear, mobility, fractured teeth or fillips, shifting of tooth positions, open contacts, abfractions, tori and posterior interferences.
Periodontal health: Recession, bleeding upon probing, minimal attached gingiva, increased probing pocket depth, furcation involvement.
Pre-Planning: Reading the charts
 Before a patient even comes into my chair, we have a process which we call pre-planning. Our pre-plan is so important because the week before, we’re going to look into that patient’s chart and review what treatment is outstanding. If anything has not been done, how are we going to move those patients into getting that treatment done and the necessity of it?
Before a patient even comes into my chair, we have a process which we call pre-planning. Our pre-plan is so important because the week before, we’re going to look into that patient’s chart and review what treatment is outstanding. If anything has not been done, how are we going to move those patients into getting that treatment done and the necessity of it?
We are going to look at medical history. We want to know what medications they are taking and if there’s pre-med needed. We need to make sure the hygiene coordinator confirms the day before with the patient that premed is needed, what they take and how much. Other considerations include:
- Are they diabetic? If so, we want to make sure that their sugar levels are good before doing treatment.
- Look at all X-rays and determine if any X-rays are needed.
- Read all correspondence we have sent out and what we have received.
- Look at all treatment done since last prophy, this way we can ask patient about treatment done.
Understand the patient’s full dental history
I want to read any correspondence that is sent to any referring doctor. If I have received any correspondence from an endodontist, I want to know what tooth had a root canal. What was the process? What did they do? If we sent them to the periodontist, what were the results? What do I need to be aware of? What treatment was done by the periodontist? I want to be up to date on everything that’s ever been done since the last time I cleaned their teeth. If the doctor did fillings or a crown, I want to make sure that those are fitting really well. I want to ensure that there is no occlusal discrepancies and no interferences.
Evaluate the medical health
Once the patient comes to my chair, if X-rays are needed, X-rays are taken first. I update medical history, if any medications are changed they are noted For example, patients that are on antidepressants are more likely to clench and grind their teeth. If they drink soda or sugary drinks, we know that is going to increase the propensity to clench and grind their teeth.
 After that, blood pressure is taken because I want to know what the blood pressure is that day in comparison to what it was the last time they came in. As a preventative system, if blood pressure is too high, we’re not going to see them in our chair. We want to know exactly how healthy their heart is because, oral systemically, we are putting a ton of bacteria into the system and it travels throughout the bloodstream and a lot of patients aren’t aware of that. We inform the patients about the risk factors of high blood pressure. We talk about oral systemic diseases and the importance of oral hygiene on a daily process.
After that, blood pressure is taken because I want to know what the blood pressure is that day in comparison to what it was the last time they came in. As a preventative system, if blood pressure is too high, we’re not going to see them in our chair. We want to know exactly how healthy their heart is because, oral systemically, we are putting a ton of bacteria into the system and it travels throughout the bloodstream and a lot of patients aren’t aware of that. We inform the patients about the risk factors of high blood pressure. We talk about oral systemic diseases and the importance of oral hygiene on a daily process.
Taking records for the outside medical community
 The other reason why we take blood pressure and update medical records is because if we have an office emergency, we can hand those charts off to the paramedic or doctor. We print the medical history forms for them with all medications so they are aware of what their vitals are then. I think that it’s very impressive to the outside medical community, and they will say “Wow, you got that done in hygiene?” If we have any positive oral cancer or external oral cancer findings we want to refer the patient out of office to the specialist. In our documentation we send any photos and measurements taken for the specialist.
The other reason why we take blood pressure and update medical records is because if we have an office emergency, we can hand those charts off to the paramedic or doctor. We print the medical history forms for them with all medications so they are aware of what their vitals are then. I think that it’s very impressive to the outside medical community, and they will say “Wow, you got that done in hygiene?” If we have any positive oral cancer or external oral cancer findings we want to refer the patient out of office to the specialist. In our documentation we send any photos and measurements taken for the specialist.
Evaluating the occlusion
Then we get into occlusion, which is the part that I love. I’m looking for wear facets. When I am looking at the joint, I am asking myself:
- What is the overall health?
- Is it stable?
- Is there crepitus?
- Is there subluxation?
- Is there deviation of the joint or the chin?
- Is there anterior open bite?
- Is there a posterior open bite?
It’s important to document normal and abnormal with the date and year so you can follow and if changes occur, you will know when. It is up to me to find out where and when the change happened, so I can relay that information to my doctor. Other tests I will do during this appointment are: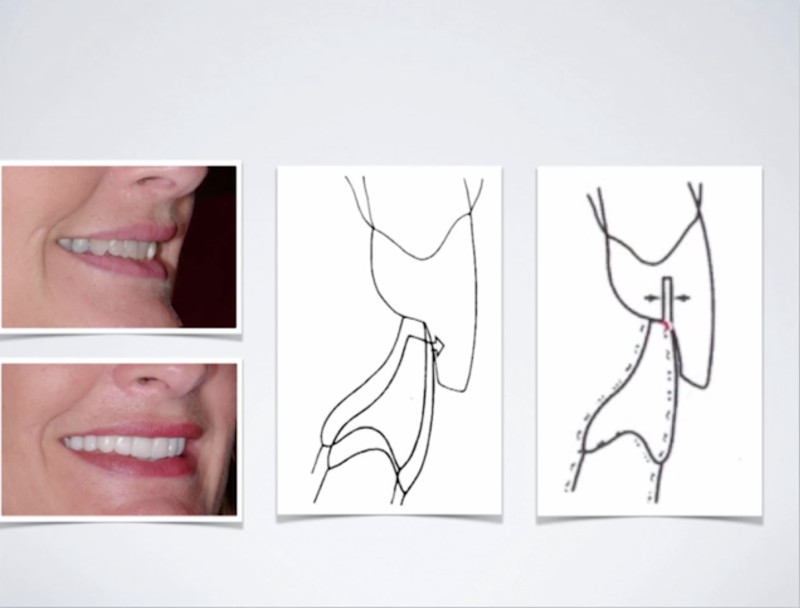
- What is the range of motion?
- Is there any mobility?
- Is there fremitus on any of the teeth?
- Do all teeth touch?
- Is there anterior guidance?
- Is there posterior disclussion on the right side and the left?
- Is the midline centered?
- Do they have any sensitivity or discomfort?
- Are the muscles quivering?
I am looking at our goals of occlusion, which are:
- Stable joints
- Stable occlusion (bite)
- Maintainable healthy teeth
- Comfortable Function
- Optimum esthetics
Understanding we don’t treat patients unless there is a symptom, our job is to access stability and inform our doctors of changes, educating our patients.
Our doctors will be the ones to determine treatment needs if any.
We want to prevent the signs of instability, understanding the signs precede symptoms. Symptoms are a result of signs going untreated. Find the signs before they turn into symptoms and the patient feels pain or discomfort. We also want to be aware that it could be very normal for them to have signs and nothing ever changes.
We want to look at periodontal factors and probe every single tooth, every single appointment. We want to get fixed measurements so we can then evaluate if anything is changing. Is the change from bacteria or is it from bite force? Understanding how mobility can increase pocket depth and when to intervene.
Reviewing oral hygiene and treatment needs
 We must review oral hygiene every single time. Making sure we are going over flossing, brushing, or any other medicaments needed, encouraging the patient to make sure that their home care is up to par. If there is any bleeding or inflammation, we want to make sure that we are educating them on the causes and repercussions. After we have reviewed that information, we will discuss any dental needs.
We must review oral hygiene every single time. Making sure we are going over flossing, brushing, or any other medicaments needed, encouraging the patient to make sure that their home care is up to par. If there is any bleeding or inflammation, we want to make sure that we are educating them on the causes and repercussions. After we have reviewed that information, we will discuss any dental needs.
Example: We have decay on the distal of 29 and it needs to have a filling in it. I’m going to talk to that patient prior to when the doctor comes in. If it’s a really large filling, I’m going to tell them there’s two choices. The doctor may fill it or they may crown it. I want the patient to know options and that the doctor will decide the treatment needs.
Prepare for the handoff to the doctor
Our role is to find and discuss options, so we can then present it to our doctors for them to discuss. The transition needs to be easy with the handoff so our doctors aren’t spending a lot of time in our rooms. If we have presented everything to the patient and doctor then agrees with treatment, then the appointment scheduling is so easy. One of the biggest problems that dentists have is time. The doctor doesn’t want to come into hygiene, spend 30 minutes in my room discussing findings. I will do that before they come in and all they have to do is come in and give the patient the treatment of choice. Knowing that the patient is already aware makes this transition very easy. Now, we can have a quick discussion about fees and time units and how we want to layout the treatment plan. Then I schedule the patient for both the doctor and future hygiene appointments, clean your room, set up for the next patient.
Ensure your hygiene team is identifying signs of instability by enrolling them in Hygienist’s Role in Supporting Complete Care Dentistry.









Leave a Reply
Want to join the discussion?Feel free to contribute!