
Airway + Dawson Dentistry through the eyes of an Orthodontist (Part 2)
This article is a continuation from an interview with Dr. Richard Roblee, a featured speaker at the 2020 International Airway Symposium. For Part 1, click here. We continue our conversation with Dr. Roblee on his overall philosophy and how airway now fits into his busy orthodontic practice.
Airway is more than sleep apnea
Kelley Richardson: Many of the doctors who come to our Airway Symposiums are looking for ways to integrate the screening and treatment protocols for airway-compromised patients. How would you advise them on practice integration?
Dr. Richard Roblee: One of the fundamental components of dentistry is to treat airway, and more importantly, to not damage it. Airway is rampant the entire gamut throughout. When we talk about current state of airway in dentistry, we are really talking about dentists referring to what we can do with oral appliances or what we can do with maxillomandibular advancements. That’s not what I’m about.
I’m focusing on what we can do to treat and prevent, not just put Band-Aids on it. Airway does not mean by any means sleep apnea. It’s far beyond that. Sleep apnea is at the end of the cycle typically when they’re starting to have comorbidity problems associated with it. When you start learning more and more, you start wondering why don’t we start preventing these issues and treating them earlier and earlier. I’m a good friend of Dr. Kevin Boyd. He’s talking about airway treatment on patients from birth to 7 years of age. We are seeing teenagers and adults with all these massive problems in old age.

The airway is all about volume. The oral and nasal cavities are the gateway to overall health. What we find in people that don’t have sleep apnea, but have airway issues, is that they may present with upper airway resistance problems and fragmented sleep. This is what gets people so fatigued with dark circles under eyes, mouth breathing and other things. We are tremendously helping their airway to develop them to their full potential, up into their 80’s. We can’t cure all problems with this, but there’s a significant part of airway problems that we can make major improvements. A lot of times, either they don’t have to wear anything or we can get them in a very conservative mandibular advancement appliance, instead of condemning them to a CPAP for the rest of their life. There’s all different levels and when people ask me, “Is this going to cure my airway problem?” If you’re like 60-80 percent of our patients, it’s going to significantly help. But the one thing I will guarantee is that you’re going to love the changes in your smile and your face. By expanding the arches, the esthetics are the added bonus.
The oral cavity is a box
Kelley Richardson: In the whitepaper you and Dr. Jerome Rose co-authored and published, The Origins of Dental Crowding and Malocclusions: An Anthropological Perspective, you conclude it’s ideal to increase jaw dimension versus extraction. How do you discuss your findings with orthodontists who have differing opinions?
Dr. Richard Roblee: It’s tricky because now we have the orthodontic specialty trying to prove that taking out teeth doesn’t cause airway problems. Well, what they’re going to find is they don’t cause airway problems, but they don’t help airway problems either. If we’re looking at helping the airway and maximizing esthetics, it’s all about arch development. Extractions don’t fit into that model, except very rarely. Certainly, I’m not condemning everybody who’s ever taken out teeth, because we all were trained that way. When we’re putting airway into the mix, we’re talking about not only improving the quality but also the longevity of patient’s lives. We give them great smiles at the same time. That’s what drives me, it’s incredibly rewarding to do that.
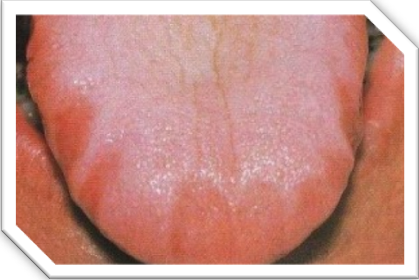 You have to think, when you take out teeth, the orthodontist is treating to the small arches. They’re not making it smaller, they’re not necessarily hurting the situation, but they’re certainly not improving it when it comes to tongue volume and opening up the airway. The way I look at it, the oral cavity is a box and the tongue is a balloon. If the box is too small, and you put the balloon in the box with lid on then, that balloon is going to fill every nook and cranny and go wherever it can. Somebody with small arches, will have a scalloped tongue. The tongue has nowhere else to go but back. The tongue is a hydrostatic muscle, which means it doesn’t change size, but it changes shape. My goal is to make the box bigger and give the balloon more room. It works tremendously well and it’s infinitely more beautiful in the end result.
You have to think, when you take out teeth, the orthodontist is treating to the small arches. They’re not making it smaller, they’re not necessarily hurting the situation, but they’re certainly not improving it when it comes to tongue volume and opening up the airway. The way I look at it, the oral cavity is a box and the tongue is a balloon. If the box is too small, and you put the balloon in the box with lid on then, that balloon is going to fill every nook and cranny and go wherever it can. Somebody with small arches, will have a scalloped tongue. The tongue has nowhere else to go but back. The tongue is a hydrostatic muscle, which means it doesn’t change size, but it changes shape. My goal is to make the box bigger and give the balloon more room. It works tremendously well and it’s infinitely more beautiful in the end result.
Kelley Richardson: I appreciate your time today. It was an absolute pleasure speaking with you. We’re looking forward to your presentation at the 2020 Airway Symposium in January.
Dr. Richard Roblee: You’re so welcome. I’ve got hundreds of cases to back all these up. So we will have a fun time, especially with the other speakers. They’re giving great medical-based evidence and I’m going to add a real world of dental perspective on how we can do this and make people more beautiful at the same time.









Leave a Reply
Want to join the discussion?Feel free to contribute!